Pierce Division efforts
Service Delivery
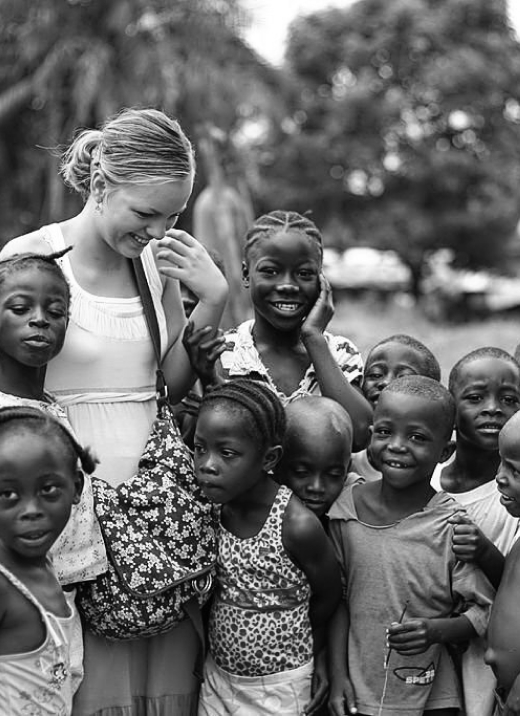
Related test goes here in this spot and this current text is just a place Global mental health delivery refers to the implementation of effective, evidence-based, timely, accessible, and affordable mental health care in settings with limited formal mental health services, with attention paid to both clinical and social dimensions. Practitioners of clinical mental health services are today “global” practitioners wherever they work. Innovative approaches to care informed by the field of global mental health to improve access to services are now a significant area of social innovation, including through the translation of lessons learned in global settings to improve access to care delivery in the US. Pierce Division faculty are engaged as leaders and advisors in mental health service delivery and capacity-building efforts around the world. They are engaged in the delivery of accessible, quality mental health care and the expansion of collaborative models of care delivery within public sector health systems and in community settings. This includes direct care as well as in advisory capacities to non-governmental organizations as well as to inter-governmental agencies such as the World Health Organization. It also includes translating best practices in global mental health delivery from global settings to the US, where 42 percent of people experiencing an acute mental health crisis cannot access care.
The need to close mental health service gaps across all contexts
Service gaps refer to poor treatment coverage as well as
to a limited range and quality of services, in all global contexts. Neuropsychiatric disorders, both common and severe, account for
approximately 16% of the global burden of disease, with the burden doubling in
the quarter century before COVID-19 and compounded by the pandemic. Neuropsychiatric
and non-communicable diseases (NCDs) are the leading causes of mortality and
morbidity and the largest contributors to DALYs worldwide. Over the past 3
decades, these numbers have continued to rise. Increasing life expectancies,
sedentary lifestyles, unhealthy diets, cigarette smoking, and the harmful use
of alcohol and other drugs have contributed to the growing incidence of NCDs.
Unfortunately, health and human resources devoted to
mental health around the globe have remained disproportionately small. Despite
the global burden of illness attributed to mental disorders being approximately
16% of total DALYs, governments globally have under-funded new mental health
services; roughly 2% of governmental budgets globally are allocated for mental
health spending. Even in HICs with many psychiatrists, a substantial proportion
of their populations lacks access to mental health care because of in-country
health inequities. The lack of equitable access and availability to mental
health care represents a failure of care delivery systems as well as of
inadequate human resources. Recurring health system gaps in resources for
mental health care delivery are further exacerbated by climate change, natural
disasters, conflicts and other humanitarian crises that disrupt and displace
populations.
Psychiatry, as a branch of medicine, has focused on the
diagnosis, treatment, and prevention of mental, emotional, and behavioral
disorders. The field can also play an important role in global mental health
and in contributing to addressing the growing burden of mental disorders in
locations with few formal services, or where access to services is poor. This
includes care in high income countries such as the US, where significant
disparities exist and where access to care is challenging. Key strategies to increase
access to, and the quality of, mental health care in all settings include
integrating mental health into primary care, increasing clinical care capacity
by training non-specialized health workers (task sharing), and using
technological tools to expand mental health coverage. A global practice of Psychiatry that bridges clinics and communities
requires the integration of categorical (emphasizing clinical diagnosis and
treatment) and dimensional (emphasizing prevention, promotion, and recovery)
approaches to care and support, provided in culturally relevant ways.
Mental health professionals can therefore serve as
leaders in clinical care delivery, training and education, research, and
advocacy to address the urgent need to expand access to mental health care and
to integrate services into primary care systems and communities. This includes
using clinical approaches as well as expanding engagement in supporting
prevention and promotion through efforts to integrate mental health care
outside of the health sector in every country, while being mindful of local
contexts. Mental health professionals have an essential role to play as leaders
and clinical experts supporting the integration of task-sharing of
psychosocial, psychological, and psychiatric interventions in collaboration
with existing primary care resources, leveraging their experience and expertise
in supervising, training, and mentoring general health workers and community
providers, as well as improving care environments and advocating for action in
other environments, such as homes, schools, and workplaces. They can also work
collaboratively as part of a broader continuum of service providers and
services across a range of allied mental health and non-specialist professions.
Short quote can go here, this length is great!

