Pierce Division efforts
Crisis Response
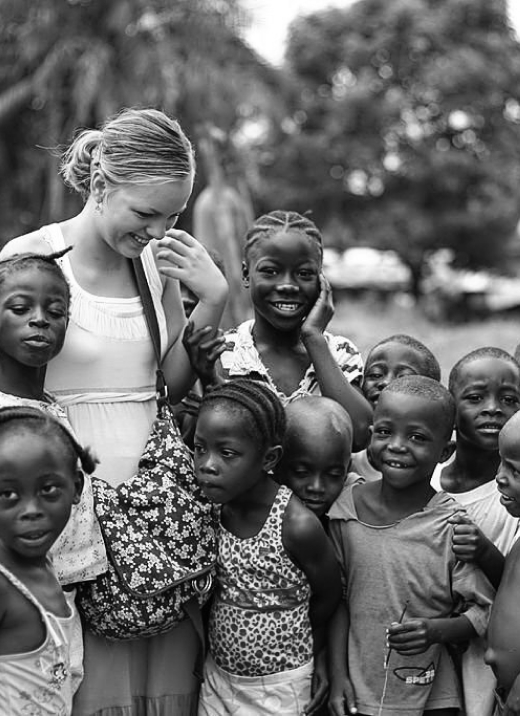
Psychologists, psychiatrists and all mental health professionals have an essential role to play in responding to natural disasters (including climate change and its evolving impacts), conflicts, and other humanitarian emergencies. Pierce Division faculty have responded as leaders to some of the major recent health crises of our time. These have included the 1994 Rwanda genocide, the 2010 Haiti earthquake response, the 2014-16 West Africa Ebola outbreak response, the Commonwealth of Massachusetts COVID-19 community contact tracing collaborative response, and the war in Ukraine. Division members co-chair the Massachusetts Psychiatric Society Disaster Readiness Committee, engage as members of the Disasters, Trauma and Global Health Committee of the Group for the Advancement of Psychiatry, and also work within the American Psychiatric Association, the American Academy of Child and Adolescent Psychiatry, and the World Psychiatric Association to strengthen partnerships that can inform societal resilience in the context of major humanitarian crises. The affiliated Harvard Program in Refugee Trauma has been a pioneer in the field of refugee mental health, delivering large-scale clinical care across disasters and conflicts, developing disaster-specific screening and response in many global contexts (Bosnia-Herzegovina, Cambodia, East Timor, Guinea, Haiti, Japan, Liberia, New York September 11th response, and in US refugee communities), training a global workforce for post-conflict and disaster recovery, contributing practical clinical frameworks for societal recovery, and many other important contributions to the field of humanitarian crisis response.
Refugee mental health in the US is an important area of engagement for a number of Pierce Division faculty.
The need to be prepared in an era of ‘polycrisis’, and to strengthen societal resilience everywhere
The 2020 to 2023 COVID-19 pandemic exacerbated the global challenge of mental health and highlighted pre-existing inequities in the availability of mental health services. COVID-19 ushered in a new era of “polycrisis,” a cross-cutting, cascading set of global challenges that spans pandemic, climate (e.g., droughts, floods, mega-storms, wildfires, extreme heat and cold) and by extension driving human migration and growing refugee emergencies, conflict over resources, and an unstable political landscape; it is now an era defined by growing complexity and uncertainty. This speaks to seemingly unprecedented global challenges, as well as to our inter-connectedness, enhanced by rapidly evolving and proliferating mobile technology. More than 15 years from the advent of the smartphone, we live in a state of balance between our ready access to information, the possible role of technology in compromising mental health, and the recognition that technology could serve mental health in innovative ways—with a new digital revolution in mental health care. Over the past several decades humanity has been adapting to rapid social change that has been enhanced by technology, most recently illustrated by the advent of artificial intelligence (AI).
Over the past decade the field of global health has increasingly integrated the concepts of mental health and psychosocial support (MHPSS), which refers to any type of local or outside support that seeks to protect or promote psychosocial well-being and to prevent or treat mental disorders, particularly in the context of emergency responses. With the aim of strengthening societal and community resilience, the integration of MHPSS skills and tools within US health care delivery systems, and their adoption by mental health care providers working in community settings, is an important enterprise endorsed by the Pierce Division.
Short quote can go here, this length is great!

